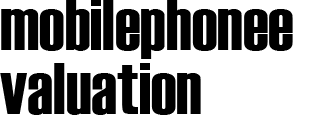
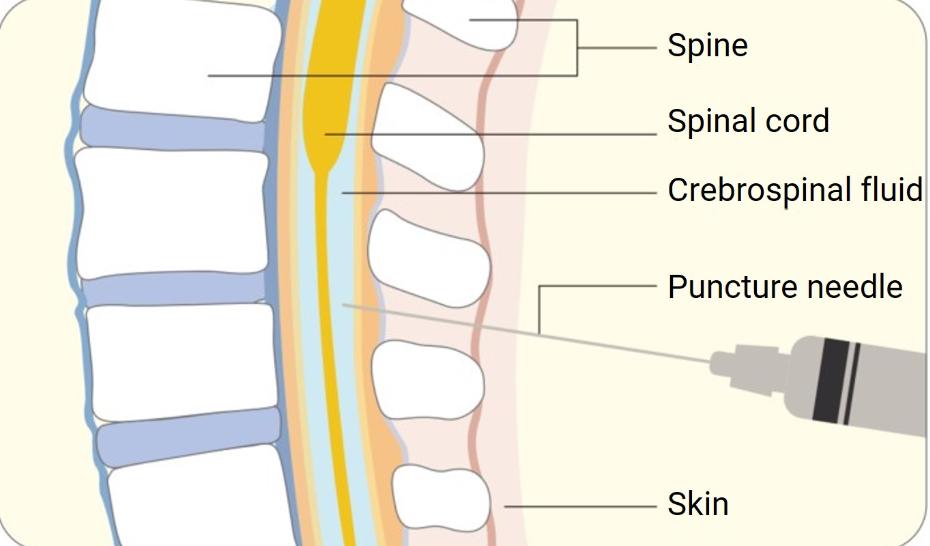
Intrathecal drug delivery involves administering medication directly into the spinal canal for pain management or to treat central nervous system (CNS) diseases. This method allows for higher concentrations of the drug at the target site with fewer systemic side effects. It’s commonly used for severe pain, spasticity, and specific cancer treatments. As intrathecal delivery gains momentum in medical practice, understanding these drugs’ safety and efficacy is crucial. In this blog, we’ll delve into FDA-approved intrathecal medications, explore chemotherapy agents used in this manner, and highlight key considerations in CNS drug development.
FDA-Approved Intrathecal Medications
Morphine
Morphine, an opioid, is a cornerstone in pain management strategies. Administered intrathecally, it offers potent relief for patients with severe chronic pain who have not responded well to other treatments. By directly targeting the CNS, smaller doses achieve effective pain management, significantly reducing the risk of side effects associated with systemic opioid use. This precise approach enhances safety, improves long-term outcomes, and provides patients with sustainable relief that supports mobility, daily activities, and overall quality of life.
Baclofen
Baclofen is essential for managing severe spasticity, often seen in conditions like multiple sclerosis or spinal cord injuries. When introduced intrathecally, Baclofen provides continuous muscle relaxation without the sedative effects that oral administration might cause. This targeted delivery improves quality of life for patients by effectively reducing muscle stiffness and spasms. With enhanced control, patients can experience greater independence, improved rehabilitation outcomes, and reduced reliance on systemic muscle relaxants, offering an overall safer and more sustainable treatment plan.
Ziconotide
A non-opioid pain relief option, ziconotide is derived from cone snail venom. Its role in intrathecal therapy is critical for patients with chronic pain who are unresponsive to traditional treatments. By blocking specific calcium channels, ziconotide provides pain relief without the risk of opioid addiction, though its usage requires careful monitoring due to potential side effects. Physicians emphasize cautious titration, multidisciplinary oversight, and individualized treatment planning to balance benefits with potential risks, ensuring patients achieve maximum therapeutic relief while maintaining safety.
Intrathecal Chemotherapy Agents
Methotrexate
Methotrexate is a cornerstone in treating certain cancers, including leukemia and lymphoma. When given intrathecally, it directly targets and destroys cancer cells in the CNS, a critical area for leukemia maintenance therapy. Despite its efficacy, careful dosing and monitoring are necessary to mitigate the risk of neurotoxicity. Physicians rely on frequent assessments, laboratory monitoring, and supportive care strategies to enhance safety, minimize neurological complications, and sustain therapeutic effectiveness, providing patients with improved long-term outcomes in oncology treatment programs.
Cytarabine
Cytarabine plays a vital role in treating hematological malignancies. Administering cytarabine intrathecally targets malignant cells within the CNS, providing an important therapeutic measure for central nervous system prophylaxis and management of meningeal leukemia. Its effectiveness is balanced by careful management of potential side effects. Clinical teams carefully monitor dosage, treatment intervals, and supportive therapies to maintain patient tolerance, maximize cancer-fighting potential, and reduce risks of neurological toxicity, ensuring comprehensive and safe integration within individualized cancer treatment regimens.
Hydrocortisone (as adjunct)
Hydrocortisone is often used in conjunction with chemotherapy agents like methotrexate or cytarabine to reduce inflammation and decrease treatment-related side effects. When administered intrathecally, it helps to protect CNS tissues and improve patients’ tolerance to intensive chemotherapy regimens. This combination reduces discomfort, preserves neurological integrity, and enhances the success of long-term cancer therapy. By preventing treatment interruptions, hydrocortisone contributes significantly to improved patient adherence, better therapeutic outcomes, and overall greater resilience during challenging chemotherapy protocols.
Other Analgesic and Anesthetic Uses
Opioids and Local Anesthetics in Spinal Blocks
Spinal blocks can provide profound pain relief during surgeries or childbirth. Combinations of opioids and local anesthetics, such as bupivacaine, are administered intrathecally to block pain signals in the spinal cord, creating a temporary numbing effect. This method provides rapid onset and effective anesthesia, reducing the need for general anesthesia and facilitating quicker recovery times. With enhanced safety, predictable results, and improved maternal and surgical outcomes, spinal blocks remain a cornerstone of modern anesthetic strategies in diverse clinical settings.
Off-Label or Compounded Intrathecal Use
Beyond approved medications, doctors sometimes use compounded or off-label drugs intrathecally for conditions unresponsive to standard treatments. This can include medications for chronic pain or neuropathic pain where innovative solutions are needed. Such use requires thorough understanding and monitoring to ensure safety, as compounded solutions lack regularized approval standards. Clinical oversight, ethical guidelines, and strict patient monitoring are necessary to maintain treatment integrity, balancing innovation with safety in the evolving field of intrathecal therapy.
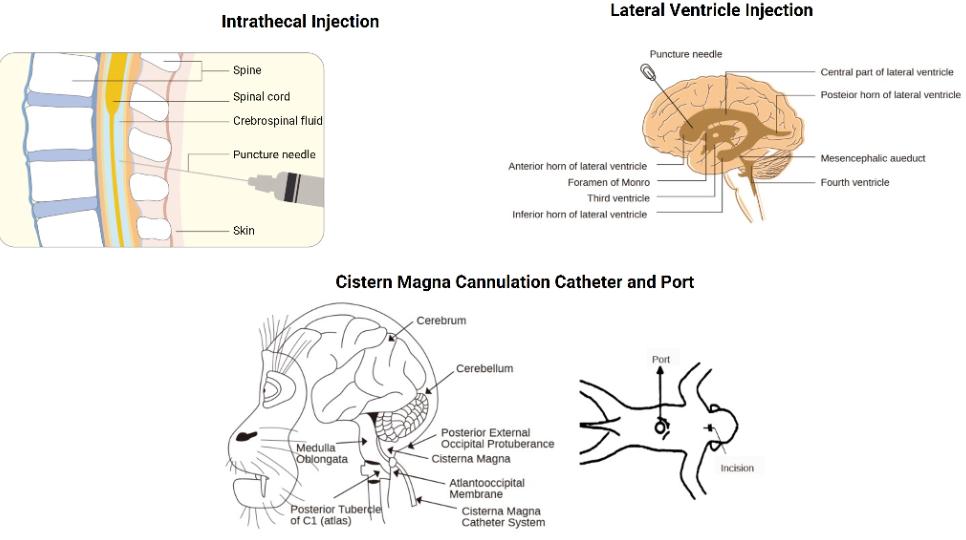
Insights from CNS Drug-Development Best Practices
Developing intrathecal drugs demands rigorous testing to ensure efficacy and safety. This involves detailed trials to evaluate not only the direct effects on the CNS but also potential systemic side effects. Ethical considerations are paramount, ensuring informed consent and patient safety throughout trial phases. Moreover, collaboration between pharmacologists, neurologists, and patient advocates is essential in forming guidelines to navigate the complexities of CNS-targeted therapy. Industry standards encourage transparency and ongoing research to refine these treatments, optimize safety, and expand therapeutic applications.
Conclusion
Intrathecal drug delivery offers a precise approach for addressing severe pain, spasticity, and CNS oncology needs. By bypassing the blood-brain barrier through intrathecal administration, it provides effective treatment with fewer systemic side effects. As research advances, new intrathecal therapies are expected to emerge, holding promise for improved patient outcomes. Awareness and understanding of these options empower healthcare professionals to leverage this mode of treatment effectively, ensuring patient safety and improved quality of life in those facing complex medical challenges.